EYE Can See Clearly
BY JOSEPH KAYS
Glaucoma is an insidious disease, as many of the 2 million Americans who suffer from it can attest.
It ambushes a person in early middle age and begins to destroy the retina and optic nerve, working from the outside of the field of vision in, so that by the time they notice a loss of vision, up to half of the one million optic nerve fibers have been destroyed.
And despite the fact that it is the second leading cause of blindness in the United States, researchers have yet to determine its cause. It is particularly prevalent among African Americans, who are five times more likely than whites to contract the disease and six times more likely to go blind from it.
Typically, the disease is marked by a buildup of pressure in the aqueous humor, the clear fluid that lubricates and nourishes the anterior, or front, chamber of the eye between the cornea and the lens. In normal eyes, the inflow and outflow of aqueous humor maintains a constant, healthy pressure. But with hypertensive glaucoma, the eye's drainage system becomes clogged, causing pressure inside the eye to build until it starts to damage the retina and the optic nerve that transmits visual information to the brain.
Scientists have historically considered this pressure to be the "cause" of the disease. But many people with the telltale degeneration in the retina and optic nerve do not have abnormal eye pressure, leading researchers to suspect that pressure is only a symptom of a more basic problem, possibly genetic.
The University of Florida has a long history of studying glaucoma, with a host of researchers in many departments searching for better ways to treat, diagnose and possibly even prevent the disease.
Trusopt Triumph
While much of this research focuses on diagnosing glaucoma before it does its damage, one UF discovery is already being hailed by doctors and patients as a major breakthrough in treating the disease.
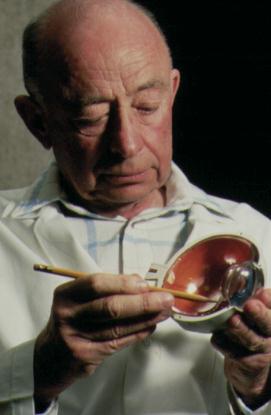 Thomas Maren got into glaucoma research by accident. As a young researcher at
the American Cyanamid chemical company in Connecticut, Maren was assigned to
lead a research team to develop a carbonic anhydrase inhibitor, or CAI.
Carbonic anhydrase is an enzyme in the body that is linked to fluid
production.
Thomas Maren got into glaucoma research by accident. As a young researcher at
the American Cyanamid chemical company in Connecticut, Maren was assigned to
lead a research team to develop a carbonic anhydrase inhibitor, or CAI.
Carbonic anhydrase is an enzyme in the body that is linked to fluid
production.
Diamox, the drug Maren's team developed, went on the market in 1954 as a diuretic to treat kidney disease, but Maren soon began hearing reports that ophthalmologists were finding it very helpful in treating glaucoma. Diamox has gone on to earn more than $1.5 billion in revenues, Maren says.
Maren left American Cyanamid soon after the development of Diamox to become a charter member of the UF College of Medicine faculty, where he chaired the Department of Pharmacology for 22 years and is now a Graduate Research Professor. As Diamox became the drug of choice for treating glaucoma, Maren assumed other researchers would figure out a way to administer CAIs topically.
The problem has always been getting the eye drops to permeate the cornea. Then the drug must reach the ciliary process, the site behind the iris where fluid is produced, and thus lower aqueous flow and pressure.
Unfortunately, Maren says, early experiments with administering CAIs like Diamox in drop form failed and it became "doctrine" that they would not work if applied directly to the eye. For a quarter century, glaucoma patients taking oral CAIs like Diamox had to suffer a host of side effects, including depression, fatigue and poor appetite.
Finally, in the late 1970s, Maren decided he would take another shot at developing a topical CAI.
"Diamox had been thought of as my drug," Maren says, "and I was getting calls from doctors all over the country telling me how distressful it was to their patients."
Supported by the National Institutes of Health, Maren first experimented in rabbits with 11 chemical compounds in search of one that would "diffuse across the cornea, get into the eye and lower pressure." One, trifluoromethazolamide, seemed to hold the most promise, but it was not good enough for clinical trial.
Much more needed to be done, but Maren was "thrown out of every ophthalmic drug house in the country and was wondering what to do next" when an executive from the pharmaceutical giant Merck called in early 1981 to invite the UF researcher to collaborate with his firm.
"Thus began a very satisfactory relationship that I believe is a model for cooperation among industry, the NIH and the university," Maren says. "Merck stayed with the project when any other company would have given up."
Merck chemists developed and, with UF pharmacologists, tested thousands of new compounds through the 1980s before settling on dorzolamide as the drug that could best penetrate the cornea and act upon carbonic anhydrase in the ciliary process to lower eye pressure.
After extensive animal and human testing in the United States, Europe and Japan, the U.S. Food & Drug Administration approved the new drug in late 1994 and Merck began marketing it under the trade name Trusopt last spring. UF holds the patent on the basic discoveries and will receive royalties from Merck.
The typical Trusopt dosage of one drop per eye three times daily is only about one-hundredth the typical oral dosage, and the only side effects patients have reported is a slight burning when they apply the drops, and a slightly bitter taste in the mouth.
Monkey See, Monkey Do
While Trusopt treats the symptoms of glaucoma, UF ophthalmology Professor William Dawson seeks the cause, or causes.
"Traditionally, physicians have thought elevated fluid pressure in the eye was the cause of glaucoma," Dawson says. "Current scientific thought, however, indicates that pressure -- while important -- may not be the basic factor in the nerve damage that eventually leads to loss of vision."
Dawson believes some forms of glaucoma may be traced to a genetic defect, since some people have all the symptoms of glaucoma but do not have high fluid pressure, and reducing pressure does not always arrest the loss of vision.
"We're looking for a genetically transmitted anomaly that interferes with the retina's ability to automatically adjust the blood circulation within the eye, resulting in nerve damage and the visual loss associated with the disease," Dawson says.
Dawson's research team has received a $2 million, five-year grant from CIBA Vision Ophthalmics, a subsidiary of the Swiss pharmaceutical giant Ciba-Geigy, to study a colony of genetically related monkeys from an island off the coast of Puerto Rico that he hopes will provide clues to a genetic abnormality that sets up the eye for later glaucoma.
The 40 monkeys in the test group are offspring of an original colony of 400 monkeys introduced to the island of Cayo Santiago in 1938, when anthropologists studying primate social behavior feared their native habitat in India was threatened by the impending war.
In the early 1980s, Dawson asked colleagues at the University of Puerto Rico's Caribbean Primate Research Center, which administers the island, if he could borrow some monkeys for a retina research project.
"Very much to our surprise, when the monkeys arrived they had a couple of human eye diseases," Dawson says. "We sent them back, but then we found their replacements had eye problems, too."
Over the next decade, Dawson and his colleagues tracked several hundred monkeys in the colony and realized that many had the same eye diseases, particularly glaucoma.
"This isolated island habitat created a `genetic bucket' of monkeys with which researchers can predict glaucoma development," Dawson says, adding that the highly matriarchal nature of monkey society has helped to control the pedigree structure of 12 generations of monkeys from the island.
Now, through controlled breeding at UF, the researchers will be able to develop even more precise pedigrees and frequency of glaucomas in future generations of monkeys. The monkey population can be expected to almost double every year, Dawson says, so researchers can track many more generations of the disease than they could in human patients. The breeding program will also enable UF to provide monkeys predisposed to glaucoma to researchers at other institutions.
Dawson says a series of non-invasive eye tests, similar to those routinely performed on humans in eye clinics, will allow the researchers to track minute changes in the monkeys' retinas and optic nerves over successive generations and treatment conditions.
Lighting The Way
One of the tests Dawson will use on the monkeys employs a new imaging technology called optical coherence tomography, or OCT, to get much-higher-resolution images of the eye.
"Until now, the use of light as a means of imaging living biological tissue has been plagued by light scattering, which limits penetration depths and results in lower image quality and resolution," says David Reitze, an assistant UF physics professor who specializes in ultrafast phenomena.
By comparing the reflected light from a continuous beam of near-infrared light transmitted deep inside the eye with an unscattered "reference" beam, researchers are developing images 100 times better than the next best technology, ultrasound, Dawson says.
"Based on our initial studies, using the system to visualize the inner-eye structure of animals, we believe this is the most accurate method we've ever had for detecting early-stage changes in the retina and the optic nerve," Dawson adds. These initial studies were funded by a grant from UF's Division of Sponsored Research.
Reitze says conversations about the medical applications of OCT arose during several visits to UF by physicist Alexander Sergeev and his colleagues at the Institute of Applied Physics in Nizhny Novgorod, Russia.
Russian scientists seeking higher-resolution underwater images for their submarines were developing OCT at about the same time as Professor James Fujimoto and a research group at the Massachusetts Institute of Technology.
Sergeev arranged for the first OCT device to be installed at UF and will continue to collaborate with UF scientists on ways to probe deeper into human tissue and to create three-dimensional images.
Ultimately, Reitze envisions using OCT with endoscopes to get high-resolution images from deep inside the body.
"This research, while basic in character, has clear and potentially revolutionary implications for the diagnosis of diseases," Reitze says. "Tissue structure, organization and content are routinely examined by ultrasound, magnetic resonance and X-ray technology. The equipment to perform these tests is expensive, large and potentially dangerous. OCT improves the resolution by a factor of 100, uses smaller, innocuous equipment and is comparatively less expensive. It is also potentially much faster than MRI or CAT technologies."
Beagle Eyes
As a young researcher at Kansas State University and the University of Minnesota in the early 1970s, Kirk Gelatt stumbled onto a litter of beagles that seemed to have an unusually high incidence of glaucoma. It turned out that a breeder had accidentally let a brother and sister mate and their offspring all developed glaucoma.
"The way this litter occurred suggested an inherited disease," says Gelatt, professor of comparative ophthalmology and former dean of the UF College of Veterinary Medicine. "Fortunately, the first time we tried to reproduce the disease, we struck gold."
Beginning with his arrival at the veterinary medicine college in 1976, Gelatt and his colleagues have used the beagle colony he had developed out of that initial litter to conduct scores of tests for a wide variety of glaucoma medicines.
"With these dogs, we've probably produced more than 70 journal articles, trained 10 graduate students and received more than $2 million in grants," Gelatt says.
While researchers like Dawson focus on the back of the eye, where the optic nerve descends from the retina, Gelatt and colleagues like Dennis Brooks, associate professor of comparative ophthalmology, explore the front of the eye.
"Changes occur in the front of the eye that damage the retina and optic nerve at the back of the eye," Brooks says. "Research on the back of the eye is currently very hot, but they are all interconnected."
The beagles -- many of whom have been raised in Gelatt's home -- are very good patients, allowing researchers to check the fluid pressure in their eyes several times a day. Also, because they begin to show signs of glaucoma as early as 12 to18 months after birth, and because dogs age faster, they are excellent research subjects.
Gelatt and Brooks believe the UF beagle colony has helped the university to become a glaucoma center, attracting top faculty and students interested in the disease.
"First we had rabbits, then we've had the beagles," Gelatt says. "The monkeys will be yet another model that we can use to close in on this disease."
Brooks says glaucoma is "much more common than most people realize" in horses, and he hopes to develop a new research thrust to study horses.
On The Front Lines
Ultimately, drugs and surgical procedures that help to relieve glaucoma in animals have to be tried on humans if the research is going to result in anything more than new ways to treat glaucoma in rabbits, dogs and monkeys.
That's where Drs. Mark Sherwood, Mary Fran Smith, William Doyle and their team come in.
Sherwood, chairman of UF's ophthalmology department, Doyle and Smith employ new surgical techniques and new combinations of surgery and drugs to treat glaucoma that no longer responds to drugs like Trusopt.
"Glaucoma is a progressive disease," says Dr. Jose Alfredo Garcia, a postdoctoral fellow working with Sherwood. "You go from drops to laser therapy to surgery. This is the place people come to when their ophthalmologist says `We can do no more.'"
And many people come to UF, where the Eye Center is treating about 5,000 patients.
Trabeculectomy, or trab, has been the standard surgery for glaucoma for a quarter century, says Garcia. Doctors surgically create a small alternative drainage pathway and filter at the perimeter of the anterior chamber of the eye to increase the outflow of aqueous humor and reduce damaging pressure inside the eye.
But sometimes, scarring around the new drain causes it to clog again. So Sherwood and his colleagues have been experimenting with drugs, many of which are already being used to treat cancer, to reduce scarring and increase the effectiveness of the surgery. Among the most successful have been mytomycin and 5-fluorouracil.
Another approach UF doctors have been perfecting is the glaucoma drainage implant. Surgeons run a tiny tube from the anterior chamber of the eye, where the excess fluid builds up, to a small plastic disc sutured to the surface of the eye.
In addition to improving surgical techniques, Sherwood's team participates in a number of clinical trials of potential new glaucoma drugs. For example, UF was one of several eye centers to test Trusopt before it was approved by the FDA.
Garcia says UF and a few other ophthalmology departments around the country are also participating in efforts to better measure glaucoma patients' quality of life through the whole range of available treatments.
"We have many diagnostic tests that we can do at the Eye Center," Garcia says, "but there is no uniform way of measuring what glaucoma or our treatments for glaucoma mean in patients' daily lives."
Working with statisticians and anthropologists, researchers are trying to develop a standard evaluation form that will question patients about everyday things like how well they see traffic signs, food labels or television screens.
"This will give us an instrument to uniformly evaluate patients from different areas of the country on a regular basis," Garcia says. "It adds a new dimension to patient follow-up."
Dennis E. Brooks
Associate Professor, Department of Small Animal Clinical Sciences, (352) 392-4700,
deb@gnv.ifas.ufl.edu
William W. Dawson
Professor, Department of Ophthalmology, (352) 392-2841,
wdawson@eye1.eye.ufl.edu
Kirk N. Gelatt
Professor, Department of Small Animal Clinical Sciences, (352) 392-4700,
gelatt.
vetmed3@mail.health.ufl.edu
Thomas H. Maren
Graduate Research Professor, Department of Pharmacology and Therapeutics, (352)
392-3544
David H. Reitze
Associate Professor, Department of Physics, (352) 392-3582,
reitze@phys.ufl.edu
Mark B. Sherwood
Professor and Chair, Department of Ophthalmology, (352) 392-3451,
sherwood@eye1.eye.ufl.edu