|
|

|
 |
|---|
Dr. Nancy Mendenhall displays disks that direct the proton beam. The gold aperture has a two-dimensional window in the approximate shape of the target being treated. It blocks protons from traveling beyond the white acrylic compensator, which fine-tunes the beam's depth to an individual patient's treatment needs. |
Basic Physics
Understanding how proton therapy works requires a brief review of basic physics. All matter, including biological tissue, is comprised of molecules with atoms as their building blocks. In each atom, negatively charged electrons orbit around a nucleus or protons and neutrons.
The goal of any radiation treatment is to disrupt the atomic structure of the cancer cells. Conventional radiation treatments use packets of electromagnetic energy called photons, or X-rays, to accomplish this goal, while proton therapy uses positively charged protons.
During treatment, doctors bombard the tumor with either photons or protons, knocking the electrons in the tumor’s atoms out of their orbits. This action, called ionization, damages cells, particularly their ability to divide or proliferate. While both normal and cancerous cells suffer this damage, a cancer cell’s ability to repair itself is frequently inferior. As a result, cancer cells sustain more permanent damage than normal cells.
The biggest difference between photon therapy and proton therapy is the degree of control doctors have over the radiation, and the side effects.
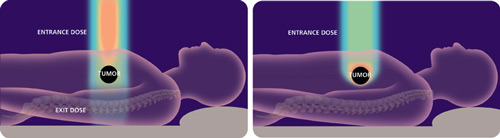
Photons enter the body at a high energy level, travel through the body to the tumor, and then exit the body on the other side, exposing all tissue in their path to damaging radiation. In contrast, protons enter the body at a low energy level and release most of their energy upon impact with the tumor.
Instead of having to balance the amount of radiation needed to destroy the tumor against the potential damage to healthy tissue, doctor’s can control the energy distribution of protons in a three-dimensional pattern, pinpointing the most power at the exact site of the tumor.
“Proton therapy has the potential to so decrease toxicity from radiation therapy that we are going to begin to harness the power of radiation therapy and effect a much higher cure rate than we have been able to achieve in the past,” Mendenhall says.
Although proton therapy has been around since the 1950s, Mendenhall says it has been only in the last decade that imaging quality has allowed doctors to exploit protons’ highly focused radiation.
“Until you can precisely delineate the borders of the tumor, you don’t want to make your radiation dose conform too tightly because you might miss the cancer,” Mendenhall says. “Protons would have been useful for only a few tumors in the 1970s and 1980s because we just couldn’t define them well enough with the imaging tools of those days. By the mid-‘90s, with high-resolution CT scans and magnetic resonance imaging, it began to make sense to precisely conform our radiation dose distribution around these better-defined tumor targets.”
And that opens up whole new avenues of treatment.
“While proton therapy is not right for every patient, it has a high rate of success in curing prostate cancer with minimal side effects,” Mendenhall says. “Thus far, the results reported for cancers in children and in cancers of the brain, lung, head and neck, eye, cervix, gastrointestinal tract, bones and soft tissues look extremely promising.”
 |
|---|
Conventional Radiation Therapy (left) exposes all tissue in its path to damaging radiation. Targeted Proton Therapy (right) releases most energy upon impact with the tumor. |
Radiation Research
As the only one of the five proton therapy treatment facilities in the United States to include a research laboratory in the same building, UF’s Proton Therapy Institute is uniquely equipped to explore new applications for proton therapy.
“Research is one of our core missions, and we’re excited about the prospects of conducting both clinical and basic research on site in our 12,000 square feet of lab space,” says Stuart Klein, executive director of the institute. “Research also will help us differentiate ourselves from other proton facilities and kind of set us apart from the rest of the pack.”
The building’s physical design will facilitate an exchange of ideas among basic, translational and clinical scientists.
As patients are treated — only one of four treatment rooms is now in use but all four are expected to be operational and treating up to 200 patients per day by 2008 — medical doctors and researchers can share ideas and strategies.
“Because of their proximity, clinical investigators can communicate in one direction with the basic scientists to say ‘We’ve got this problem and we don’t understand what causes it. Can you figure this out and tell us what’s happening here?’” Mendenhall says.
The basic scientists can then tackle the problem and try to
recreate these issues in the lab. Once they understand the pathway, they can propose solutions to the translational researchers who then ask the clinical investigators to test the treatment.
“So, we get this circle of conversation going, and the circle can go the other way, too,” Mendenhall says. “The basic scientist may find something curious about a mechanism and ask the clinical investigator for advice on how to modify and enhance it and then ask ‘What happens here? Is it good or bad?’”
Numerous UF scientists are looking at the application of proton therapy to their particular specialty. For example, proton beam therapy is especially desirable in the eye, where precise delivery is so important, according to Dr. K.V. Chalam, associate chair of ophthalmology in the College of Medicine-Jacksonville.
“With protons we can deliver energy at a determinable depth and target tissue hidden underneath healthy layers of eye tissue — a technique useful in treating a common blinding complication of age-related macular degeneration,” he says. “Proton therapy also has been used successfully to conservatively treat melanomas in sensitive locations such as close to the optic nerve.”
Dr. Sameer Keole, assistant professor of radiation oncology, hopes to use protons to better protect pediatric patients with brain tumors.
“For these patients, we often have to treat the entire brain and spine to prevent tumor spread,” he says. “With photons (X-rays), the beam exits through the front of the patient, giving unnecessary dose to critical structures, including parts of the esophagus, thyroid gland, major blood vessels, kidneys, lung and heart. With protons we lower the radiation dose to all of these structures.”
 |
|---|
Protons are extracted from water through electrolysis, injected into a cyclotron and accelerated to nearly the speed of light. Then they're guided through a pipeline with magnets into a treatment room.
|
Keole is developing a study to conduct cardiac MRIs on pediatric patients receiving proton radiation to the spine.
“By doing these studies both before and after the radiation is delivered, we will see if there is any evidence of cardiac damage,” he says. “Then we’ll compare this group to patients treated in the past with photon radiation to see if there is a difference in cardiac function.”
The brain offers some of the most promising areas for improved treatments, says Dennis Steindler, director of UF’s McKnight Brain Institute.
“We have a particular interest in brain tumors, and the proton beam has many applications in that area,” Steindler says, “so we would be interested in using the beam to test new therapeutic approaches in animal models.”
Proton therapy also offers opportunities to study regenerative medicine.
“We have a very strong regenerative medicine group that’s interested in cell and tissue engineering,” Steindler says. “We want to use models that the facility and that group of clinical investigators already have in hand to help us look at ways in which we can further enhance tissue repair following this type of radiotherapy.”
Steindler is particularly excited about a collaboration the Brain Institute has with the Kennedy Space Center and NASA to look at the effects of cosmic rays on astronauts during long-distance space missions to places like Mars.
“We’re interested in what effect these cosmic rays have on brain cells and, in particular, adult brain stem cells,” Steindler says. “We want to pursue Earth-based cosmic ray exposure models before moving to the International Space Station or the shuttle.”
McKnight researchers have already been conducting some experiments at the Brookhaven National Laboratory in New York, but now they will be able to move this work to the Jacksonville facility.
“It’s beyond the preliminary stage. We’re well into experimental design,” Steindler says. “I think that part’s pretty cool, myself. It’s to protect our astronauts as well as use the facility to figure out ways to research the potential radiation risk that we’ve all heard about in long-term space missions.”
Steindler adds that while these radiation exposures probably do not have the potential to generate full-blown cancer, they may certainly make tissue susceptible to cancer.
Mendenhall says the research and treatment being conducted at the Proton Therapy Institute will generate massive amounts of data that can also inform the business end of health care.
“If we’re comprehensive in our data accrual and we have a continuous longitudinal database, we can use this to tackle healthcare costs, look at the comparative cost of different treatment strategies and look at cost of care in not such a fragmented way,” she says.
The questions are many and will generate new research topics. What are the long-term costs of radiation vs. surgery in terms of management decisions? How do complex factors like treatment of complications, treatment of recurrences, treatment of anxiety, loss of family income during long-term treatment affect broad healthcare issues?
“I think we’re creating a real model for not just multidisciplinary research but multidimensional research,” Mendenhall says. “We want to make the most efficient use we can of our patient resources and of our facility resources to do the very best research we can to help patients everywhere.”
Ultimately, Mendenhall says, all of this research leads back to quality patient care.
“There is an expectation from society that we not only provide the best in care to our patients but that we continue to search for better ways of doing things,” she says. “We’ll have an impact way beyond this campus, way beyond the walls of the Proton Therapy Institute. Our impact will be felt across the country by cancer patients.”
Nancy Mendenhall
Medical Director, UF Proton Therapy Institute
(904) 588-1800
mendenan@shands.ufl.edu
K.V. Chalam
Associate Chair, Department of Ophthalmology
(904) 244-9361
kchalam@jax.ufl.edu
Sameer Keole
Assistant Professor, Department of Radiation Oncology
(904) 588-1800
keole@ufl.edu
Dennis Steindler
Director, McKnight Brain Institute
(352) 392-0490
steindler@mbi.ufl.edu
Related Web site:
www.floridaproton.org