Beyond Bones
Advanced imaging technologies allow doctors to see inside
the human body like never before
BY JOSEPH KAYS
|
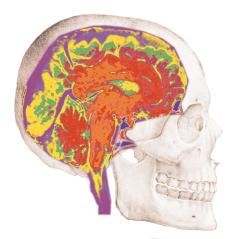
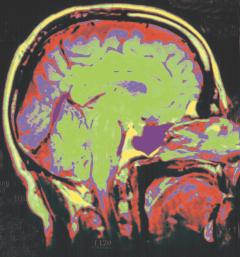
This artificially colored NMR image of the brain, superimposed on a classical drawing of the skull, was produced using a 3 Tesla machine operated jointly by UF's Shands Hospital and the Gainesville VA Medical Center. The machine is one of only seven such devices currently in use in the United States. |
Image a head using computerized tomography (CT), nuclear magnetic resonance (NMR), positron emission tomography (PET), single photon emission computerized tomography (SPECT) or a host of variations on these imaging technologies and you see tissue, blood vessels, nerves, emotions, senses, thoughts.
In the last quarter century, faster computers, more powerful magnets and more precise radioactive isotopes have offered doctors ever-clearer windows into the human body, allowing them to diagnose illnesses earlier and better, without ever having to pick up a scalpel.
``We have had a heyday and I don't know when it will stop,'' says UF radiology Professor Jon Williams. ``There's absolutely no question we have the ability now to identify tumors we simply couldn't even see 15 or 20 years ago. These are things we used to find months or even years down the line, or in a post-mortem examination.''
While current technology gives doctors astonishingly clear ``photographs'' of the body, the future is focused on functional imaging, real-time ``movies'' of physiological events in action.
Researchers and doctors already are experimenting with new or improved imaging technologies that allow them to see parts of the brain ``light up'' in response to specific stimuli, such as a noise or a pin prick.
This information will make it easier for surgeons to identify healthy tissue so
they can plan surgery for everything from tumors to epilepsy more accurately.
Wired For Sound
|
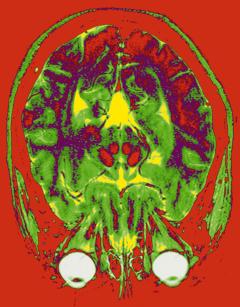
| MRI allows doctors to make high-resolution images of human tissue like the brain pictured here from virtually any angle. |
|
The application of nuclear magnetic resonance to medical imaging is one of the great advances of the last quarter century. Since magnetic resonance imaging machines first arrived in hospitals in the early 1980s, researchers have concentrated on improving the already extraordinary images they produce.
The challenges to building better NMR diagnostic tools fall in two areas, says UF radiology Professor Jeff Fitzsimmons: ``If you want a high-resolution image to see smaller and smaller abnormalities, you need either higher-field magnets or better antennae, or both.''
A third element, critical to the next generation of functional NMR scanners, is extremely fast computers able to simultaneously translate the millions of bits of information generated by the magnets into pictures on a monitor.
Fitzsimmons — who has an eclectic mix of training and education in electrical engineering, psychology and computer science — says he and other UF researchers began pursuing the idea of developing better antennae for receiving the NMR signal even before UF's first MRI machine was installed in 1983.
``We looked at the various aspects of the MRI systems for areas where we thought we could produce a noticeable improvement,'' Fitzsimmons says, ``and we realized that we could improve the equipment's performance a lot by redesigning the antennas.''
The antennae Fitzsimmons and his colleagues developed are called coils, arrays of copper tubing and copper tape designed to fit snugly around the area to be imaged, be it a skull, a breast, a shoulder or a knee.
``Coils are essentially better antennae for picking up the radio waves the body produces when it is placed in a magnetic field,'' Fitzsimmons says. ``These coils can improve the performance of the machine by as much as 40 or 50 percent.''
Fitzsimmons says that in the pioneer days of MRI in the early 1980s, ``the industry wasn't attuned to building MRIs for animals, much less humans. They were building them for test tube-sized samples.
``We pretty much had to design our own coils because there was nothing available commercially,'' he adds, pointing to a crude-looking piece of copper tubing gathering dust on his desk. ``That was our first coil. It was designed to fit around your neck.''
Today, coil designers spend considerable time theorizing about the configuration of coils and creating computer models before initial test models are constructed at a workroom in the MRI facility that looks like the spare parts room for the Crash Test Dummies.
Old football helmets laced with copper tape, transistors and capacitors sit on shelves next to similarly arrayed tubes and cuffs of various sizes.
``Over the years, we've learned ways to get even more signal information out of the body by using an array of coils,'' Fitzsimmons says. ``Some wrap around a body part; others are strung out along a body part like the spine.''
While the coils may appear crude now, sleeker versions are likely to be
included with future MRIs, Fitzsimmons says.
Diagnostic Attraction
|
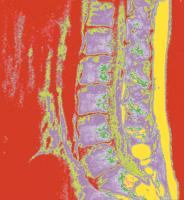
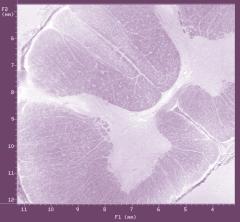
Using a 14 Tesla NMR microscope, researchers at UF's
Center for Structural Biology image damaged spinal cords and how they respond
to novel treatments.
|
UF's partnership in the National High Magnetic Field Laboratory has created new opportunities in the second part of the NMR equation, higher-field magnets.
``The main reason for pursuing high fields is that the NMR signal is more energetic at higher fields,'' Fitzsimmons says. ``We can make incremental increases in performance with better coils, but to get a dramatic increase, we must get higher magnetic fields.''
While the research currently going on at the NHMFL's main site in Tallahassee focuses on reaching the highest-possible fields (currently more than 33 Tesla), it holds significant long-range impact on medical imaging, Fitzsimmons says. Tesla is a measurement equal to 20,000 times the Earth's magnetic field.
``The magnet lab has been very successful at building very-high-field magnets, but they use very small bore size,'' he says. ``The greatest technical challenge is to reach the high fields. Once reached, extending bore size is expensive, but not as great a challenge.''
A $13.3 million grant from the Department of Defense to equip the UF Brain Institute includes several million dollars to build and install a 12 Tesla MRI unit for animal research. With a magnetic field 240,000 times that of Earth's, the unit will be capable of generating the highest resolution images yet of chemical changes in the living brain.
``This powerful new scanner will enable scientists to obtain a whole new perspective on the biochemistry of the brain and spinal cord,'' says Thomas Mareci, director of the Center for Structural Biology in UF's College of Medicine. ``Unlike standard diagnostic MRI units, which construct images based solely on the hydrogen nuclei, the 12 Tesla model will also create pictures of the cellular molecules containing other important nuclei, such as carbon, nitrogen and phosphorus.''
The third element in better NMR is numbers crunching, Fitzsimmons says.
``One of the most exciting things we're doing is functional brain imaging, a method whereby we can look at brain activity in real time,'' he says. ``We can detect very tiny changes in signal intensity caused by a particular stimulation.''
All of those signals coming out of the patient in the magnet could easily overwhelm even the fastest computers, so UF computer scientists developed a mathematical way for computers to process thousands of computations simultaneously.
A team led by computer science and engineering Professor Gerhard Ritter is working with the Air Force and Lockheed Martin to develop a hardware/software system called parallel algebraic logic (PAL) that supports computer vision at supercomputer speed with desktop size and price. The PAL system packages 9,216 processors into a computer smaller than the typical desktop machine.
Storing digital images presents other challenges and opportunities, says radiology Professor Williams.
By recording most medical images electronically, doctors have much greater ability to manipulate them for things like contrast and brightness, and ``there's no such thing as a lost film,'' Williams says. Doctors throughout the hospital and around the world will be able to access a patient's images with the punch of a computer key.
But all those digital images take up a lot of disk space. UF is considering a
picture archiving and communications system (PACS) that can store 37 terabytes
of information — 37 million times the capacity of a typical desktop
computer's hard disk.
Combining Approaches
|
How NMR Works
The basis of NMR is that a strong magnetic field applied to randomly spinning protons inside the atoms of the body, particularly hydrogen, will cause them to line up and spin in the same direction, like an army of tops. A radio signal beamed into the magnetic field knocks the protons out of alignment and as they fall back into alignment they release energy in the form of radio waves. The amount of energy released and the time it takes for the protons to line up again is unique for different tissues in the body, so a computer can take this information and create an image of that tissue.
photo from: GE Medical Systems |
As new imaging technologies have come on-line over the years, one might think that they superseded earlier technologies, but UF imaging experts say the different approaches actually complement each other.
``X-rays are excellent on hard tissue like bone, whereas magnetic resonance doesn't do a good job on bone,'' says Mareci. ``Magnetic resonance is much better for soft tissue, and the nuclear technologies are much more chemically specific.''
``When magnetic resonance came along, it was being used for just about everything and looked like the death knell for computerized tomography,'' adds Williams. ``But it turns out that while it probably has replaced CT for much of the brain and for a lot of musculoskeletal and soft tissue, it is lousy for bone, because there's no signal from bone.''
UF researchers are currently working with Ohio-based SMV of America to merge the capabilities of a nuclear medicine camera and positron emission tomography (PET) in a lower-cost scanner that can detect cancerous tumors as small as four millimeters in diameter.
``The result is one piece of equipment that requires less space to operate, is affordable and can provide health-care professionals with the ability to detect cancers that can't be 'seen' by standard scanning methods,'' says Dr. Walter Drane, director of nuclear medicine at Shands Hospital and a professor of radiology.
Both the PET scanner and the nuclear medicine camera have distinct capabilities critical in the detection and treatment of cancer, Drane says.
The new nuclear camera-PET scanning machine hybrid developed by Drane and his colleagues costs less than $500,000 — a substantial savings when compared to the $6 million it costs to establish a PET scanning center alone.
This lower-cost PET scanner gives more physicians the ability to detect tumors
before any changes in anatomy occur. It also enables them to determine the
effectiveness of chemotherapy and radiation, recurrence of cancer after
treatment and the point of the cancer's origin when the disease is not
visible by other scanning devices.

|
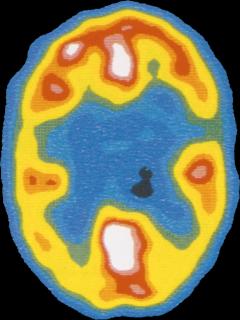
| UF epilepsy researchers use single photon emission computerized tomography (SPECT) to record seizure activity in the brain. |
``The first signs of a tumor may be that the fat plane in a certain area of the body is distorted. We can see a discrete mass or lump but often not until the tumor is about a centimeter or larger. By that time, it could easily have spread to other areas,'' Drane says.
Unlike X-rays, CT scanners or MRIs, PET does not rely on visible changes in the body's anatomy. It works by tracking the movement of radioactive glucose — the food tumors feed on. Sugar is used by the brain and stored by the liver to be used in various metabolic processes, Drane says. If cancer is present, these processes are interrupted.
``Cancer does not obey the body's natural processes. A tumor says, 'I'm growing and I need the glucose, I need it all the time and I am taking all the sugar,''' Drane says.
Once the radioactive sugar is injected, it heads to the cancer site, sending
off signals called positrons as it moves through the body that are picked up by
the PET scanner.
From ``Telescope'' To ``Microscope''
If the work Fitzsimmons and the other people who work with human NMR machines do is at the ``macro'' level, then the work Mareci and the scientists at the Center for Structural Biology do is at the ``micro'' level.
 ``You can think of the large-bore, 3 Tesla MRI machines that we put people
into as telescopes,'' Mareci says. ``We work with small-bore, 14 Tesla
machines that are the equivalent of microscopes.''
``You can think of the large-bore, 3 Tesla MRI machines that we put people
into as telescopes,'' Mareci says. ``We work with small-bore, 14 Tesla
machines that are the equivalent of microscopes.''
Mareci and his colleagues have been using this unique NMR microscopy to image spinal cord tissue and determine whether treatments like fetal tissue replacement can repair damaged spinal cord tissue.
``When we look at a piece of damaged spinal cord with a 14 Tesla NMR microscope, we can very clearly see structural differences in the white and gray matter that makes up the spinal cord,'' Mareci says. ``Now we are using our NMR microscope to study injury and whether inserting fetal tissue into the damaged area can cause any kind of regrowth.''
Ultimately, Mareci says, the ``microscopic'' research conducted on tissue samples in test tubes and laboratory animals may lead to treatments for human spinal cord injuries that result in the patient regaining at least some control of lost bodily functions.
For doctors like Williams and William Luttge, director of the UF Brain Institute, whose careers have spanned the transition from conventional X-rays to new imaging technologies like NMR, memories of the practice of medicine without such clear images are sobering.
``You go back and look at some of the old images and say 'How in the world did I ever make the diagnoses I made,''' Williams says. ``Seeing what we have now, it is truly remarkable.''
Luttge adds that ``a world without modern medical imaging would be a pretty depressing place to live in.''
``We would be in the medical dark ages. We would have to cut people open a lot more often, and a lot more extensively, to just get an idea of what their problem was,'' he says, ``and even then we'd never be able to match the diagnostic and image-guided power and resolution we now enjoy.''
Walter Drane
Professor, Department of Radiology, (352) 395-0105, dranew@xray.ufl.edu
Jeffrey Fitzsimmons
Professor, Department of Radiology, (352) 376-1611, x5072,
jfitz@ufnmr1.health.ufl.edu
William Luttge
Director, UF Brain Institute, (352) 392-3383, luttge@cortex.health.ufl.edu
Thomas Mareci
Director, Center for Structural Biology, (352) 392-3375,
thmareci@csbnmr.health.ufl.edu
Jon Williams
Professor, Department of Radiology, (352) 395-0291, williamsj@xray.ufl.edu
|
UF: An Imaging Pioneer A long history in medical imaging and recent collaborations such as the UF Brain Institute (UFBI) and the National High Magnetic Field Laboratory (NHMFL) have elevated the University of Florida to a position among the top institutions in the world in this field. ``In my estimation, we are in an excellent position to be one of the world leaders in all aspects of imaging science, with a particular emphasis placed on biomedical imaging,'' says Dr. William Luttge, director of the UF Brain Institute. ``The enthusiastic involvement of research faculty from all across our campus should permit us to successfully tackle a wide range of problems too complex for most other centers.'' Researchers from the University of Florida were pioneers in magnetic resonance imaging. Physicist Raymond Andrew, who came to UF from the University of Nottingham in 1983, was one of the first scientists to apply nuclear magnetic resonance to medical imaging. The Journal of Magnetic Resonance and the Journal of Magnetic Resonance in Medicine were both founded at the University of Florida and UF had the first MRI machine in the state. One measure of UF's prominence in the imaging field is the amount of research money awarded to the university in recent years to develop and apply new imaging technologies. Luttge says the university's imaging research capabilities clearly had a positive influence on the Department of Defense's decision to commit more than $30 million to building and equipping the nation's most advanced Brain Institute at UF. This institutional strength is also reflected in the National Science Foundation's decision to award the $100 million NHMFL to a consortium of the University of Florida, Florida State University and Los Alamos National Laboratory. ``In my estimation, UFBI and NHMFL have both clearly benefited by their association with one another,'' Luttge says. ``In each grant, the facilities and cooperative ventures of both programs, as well as other imaging science programs at UF, have been emphasized in the application materials.'' |
|
| |

| |
|