|
|
 Simulators Let Medical Students Make Meaningful Mistakes Without Permanent ConsequencesBy Melanie Fridl Ross I can truss a turkey. As a kid I was the Queen of Counted Cross-stitch. I've even been known to hem a pair of pants or two. So as I sit in front of a computer screen to try my hand at suturing a gaping wound using the latest medical simulation project to swing into action at the University of Florida, I think, "Just needle and thread. How hard can it be?" Then my cyber "patient" starts bleeding out. As a clock ticks off the seconds, I attempt to maneuver a handheld gizmo known as a haptic device that operates a virtual stainless steel needle. First I grasp the needle, a curved sliver of silver that skitters away on my first tries. Finally, I catch a tight hold. Then, twisting my wrist like a circus contortionist, I approach the wound. I actually feel resistance and then a slight pop as the skin yields to the needle, which pushes through to the interior wall of the gash. I manage to repeat the move, and the suture thread flows, gently tugging one side of the wound closed. But when I go to make my second stitch, I end up with a zigzag look with a distinct Frankensteinian flair. The computer calculates my performance, listing the number of stitches and their size and distance. It's obvious I won't be trading poultry for patients anytime soon. Flying SoloPhysicians-in-training at the University of Florida who want to practice the art of suturing will soon be more likely to head to a simulation lab than to make the traditional trip to the grocery store for a package of pigs' feet or a bag of oranges. There they will try their hand at closing incisions and stitching together the ends of blood vessels on a screen, long before they attempt it on real patients.
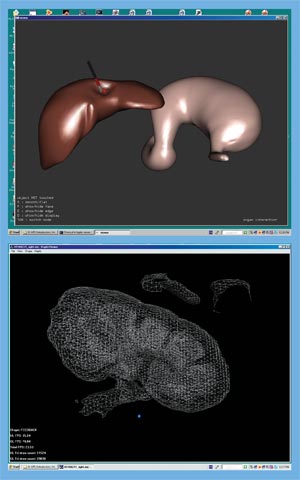
At the heart of this approach is Sergei Kurenov, who’s taken his expertise as a developer of flight simulators back in his native Russia and as a member of the Soviet-American team that helped place Microsoft Word on the Russian market and put it to use crafting simulation programs for surgery at UF’s College of Medicine. Kurenov, who is with the Department of Surgery, is just one of many researchers campuswide who believe the future of learning for health-care practitioners will be increasingly simulator-based. Major advances in computing, virtual reality and microengineering have helped make simulation a new frontier for health education and research. “The medical profession is starting to come to realize the benefits of simulation, which the military and other fields have already latched onto,” says Benjamin Lok, an assistant professor of computer science at UF. “The savings and the potential for learning are completely untapped right now. That’s where UF has the potential to get ahead of the game very quickly. “It’s only been recently that we’ve arrived at a crossroads where the technology has gotten to the point where it can provide true value to the medical community,” he adds, “and secondly, the medical community has become more technically savvy. These advances are out of necessity, but also timing is playing a role. For a long time, computers couldn’t produce anything that would be of value to medical students. That time has changed.” Only in the past decade, for example, have engineers hit on the mathematical equations necessary to simulate the resistance and flexibility of soft tissue, Kurenov says. Using a haptic device, students can feel the sensation of probing a sheet of collagen, bouncing along its surface, trampoline-like. They can poke a kidney, then watch a 3-D model rotate across the screen as the computer’s cursor weaves in and out of key structures. Simulation will allow students and residents to practice procedures outside the operating room in an objective manner many times, and to be scored on their performance, says UF surgeon Juan Cendan. “For pilots, simulation is de rigueur; they have to have gone through these things to be able to fly an airplane,” Cendan says. “Certainly surgeons are in that same category of performing very dangerous, high-stakes procedures. Practicing outside of the operating room allows us to judge when a student or resident is ready to try a procedure on a patient, and at some point we think it’s going to be very important for credentialing. You will want to know that your surgeon can at least do this on a computer simulator before he tries it on Aunt Mary.” Today, simulation is in full flower at the Health Science Center. Nursing students start IVs on “trainer” arms. Plastic heads, their mouths agape, await the probes and drills of dental students. Emergency medicine and anesthesia residents sharpen their critical thinking and resuscitation skills on mannequins in extremis.
As pervasive as it is now, the technology is only expected to grow in importance because of the confluence of several interrelated imperatives: • the recognition that medical errors represent a fundamental problem that demands an outside-the-box solution; • the need to train health science students as part of multidisciplinary teams; • the “unevenness” of the training experience, which makes it difficult to expose students to enough patients with the breadth of problems they will need to master before entering practice; and • the growing ethical consensus that real-life patients are not merely a commodity for indiscriminate use to advance teaching objectives. Of course, simulated education in all its forms — mechanical, interactive computer- and virtual-reality based, or involving standardized patients, trained actors who simulate symptoms of various ailments — will never replace the “see one, do one, teach one” experience gained at the side of a seasoned faculty member. But with far more practice on a simulator under their belts, HSC students of every flavor will be that much better prepared when they finally encounter a patient. “I think the future of learning is going to be simulator-based,” says Robert Watson, senior associate dean for education in the College of Medicine. “I believe that the providers are going to have to be able to demonstrate that they have mastered a skill before they attempt it on a patient.” This conviction, coupled with major advances in mathematics, computing, biomedical engineering, virtual reality and microengineering, has helped make simulation a new frontier for health education and research. “All six deans (at the Health Science Center) share my belief that after research space, this is our next greatest need — a high-tech, interdisciplinary teaching environment where the student, the patient and the evidence-based information are brought together for real-time learning,” says Douglas J. Barrett, senior vice president for health affairs. Teaching Tools
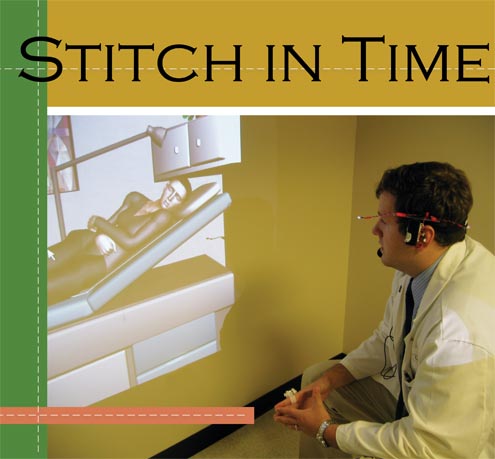
Like all medical students, Colin Brown will never forget the first time his patient coded. It was during his third year of medical school. The patient developed “a weird arrhythmia” Brown didn’t recognize. “What do you want to do?” asked his professor. Brown chose to give a certain medicine. It was the wrong call, and the patient immediately started going downhill. Brown felt overwhelmed by his confusion, yet enlightened. “It’s a wake-up feeling,” recalls Brown, now a post-doctoral researcher in anesthesiology. “You see where you went wrong and it all makes sense.” His experience speaks volumes about the power of simulation as a teaching tool. Because in this case, the fact that Brown’s patient was a 6-foot-long mass of plastic and wires didn’t seem to detract from the lesson. “How do we bridge the gap between the lecture hall and the patient?” Brown says. “(Without the simulator) the jump would have been even longer and more unforgiving. It’s a great stepping stone.” In the mid-1980s, UF anesthesia faculty J.S. Gravenstein, Michael Good, Samsun Lampotang and others pioneered the development of the Human Patient Simulator, today the most advanced and widely used whole-body device in the country. The university licensed the simulator technology to Sarasota-based Medical Education Technologies Inc., which has sold hundreds of the $160,000 plus devices to hospitals, medical and nursing schools, community colleges and military bases worldwide. The lifelike mannequin — nicknamed Stan, short for Standard Man — is programmed to mimic an array of illnesses, including emphysema, heart failure and abnormal heart rhythms, and respond to injected medications, changes in ventilation and other interventions. As an educational tool, simulation’s experiential approach is hard to beat, says Tammy Euliano, an anesthesiologist who handles most of the teaching duties involving the Human Patient Simulator. “If you asked most medical students, the things that stick the best are the things they learned at the bedside … they remember that forever, and the disease next to it in the book they don’t remember at all,” she says. Making meaningful mistakes without permanent consequences is especially powerful, Euliano adds. “In real-life emergencies, we can’t let students do much,” she says. “This technology gives us the opportunity to simulate acute incidents, let the student flail and learn from that. And then we can in a very reproducible way say, ‘All right, back up, start over, here’s what you missed, try again,’ which you could never do in real life — the incidents are just too rare for anyone to get two tries.” Keeping patients out of harm’s way is a key driver of the recent interest in simulation. Five years ago, the Institute of Medicine produced its seminal report, “To Err is Human,” sounding the alarm on medical errors in health care. But to really reduce errors, Watson believes, it’s necessary to go upstream and provide better training to health professionals in basic skills and, just as important, to assess how well those skills have been learned. This is true not only for students but also for current practitioners. “For any skill, I really think you ought to have done it at least 10 times on a simulator,” he says. “Every one of the competencies I think you could help teach and, more importantly, you could objectively, reliably and validly evaluate.” Virtual FutureWith all its possibilities, the technology still has limitations. Many are technical: the machines break down; “skin” can be punctured only so many times; the realism is not quite there. The limitation that a simulation center might best address, Euliano says, is inefficiency. She trains students in groups of three, with another nine looking on, waiting their turn. At that rate, it takes a long time to accommodate 100 students in a single medical class. She and others envision a simulation center that would include a small auditorium where every student has a handheld device that reflects the mannequin’s vital signs. That would help engage onlookers until their turn. In another activity, teams of health-care workers would watch a real-time simulation and compete to identify errors through a computer interface. The center’s crown jewel would be a large auditorium with the ability to project any one of several environments — a hospital operating room, an emergency room, the site of a mass casualty accident or bioterrorist attack. Students or experienced practitioners taking part in continuing medical education would be present to deal with a critical event. The scene would be televised to an audience of peers, who would vote electronically on what to do next. The instructor would tally the vote and demonstrate the outcome for each course of action. For all these learners, a virtual library of information will literally be at their fingertips. With one click on a laptop or handheld device, relevant patient histories, scans, lab results and scientific literature will be available for real-time consultation. Computers are expected to play an even larger role in the future through virtual reality simulations. UF medical college faculty have been working with the Department of Computer and Information Sciences and Engineering in the College of Engineering and colleagues at the Medical College of Georgia to develop a “virtual patient” students can interview. Led by Lok, computer scientists and physicians scripted a scenario involving a virtual character, “Diana,” experiencing abdominal pain. In a 10-minute virtual reality experience, medical students use speech and gestures to carry on an amazingly lifelike conversation with the life-sized Diana, who is displayed on a mock examination room wall using data projectors. The system also tracks the user’s head and hand positions. Students can point at or even shake virtual hands with Diana, using gestures they would naturally use with human patients. And preliminary studies of gaze behavior have shown that students maintain eye contact with Diana in the same way they would while talking to real people. The approach is still years away from routine use, Lok says, but he feels confident UF can make a name for itself with this technology. “This is how we can be different from every place that has standardized patients in the world,” Lok says. Lok symbolizes the collaborative energy that’s being directed toward simulation at UF. Nowhere is that more evident than in the Department of Surgery, whose chairman, William Cance, has championed the virtual character project and other collaborations with the College of Education, the Department of Biomedical Engineering, the Digital Worlds Institute and the Malcom Randall Veterans Affairs Medical Center. Efforts include creating programs that, for example, stack CT images from actual patients to reconstruct a 3-D image that enables physicians to glimpse the size and reach of a sarcoma wrapping itself around a patient’s hip — something that might be impossible to visualize otherwise. Kurenov also has tinkered with a new surgical suturing device called an Endostitch, machining the tool’s actual handle onto the computer’s haptic device and creating a program that models how the instrument works, so surgeons can practice. Other simulation efforts involve developing programs that practicing surgeons can use to try a rare operation they haven’t done before, or one they have not done in a long time. “I think that given the breadth of excellence at UF across its different colleges we can forge collaborative interactions that will allow us to move to a leadership role (in simulation), as Dr. Lok is already demonstrating with his virtual characters,” Cance says. “The critical step is having the interdisciplinary collaboration that can advance the field much more quickly by virtue of the expertise we have in multiple different areas.” It’s a grand vision that’s not too wild a leap for an institution that, after all, was there at the beginning. “We used to be light-years ahead of everyone else,” Euliano says. “Now everybody is catching up. If we got a simulation center soon we certainly have the critical mass here to move forward. I think we could really do amazing things to improve tomorrow’s health care.” Tom Fortner contributed to this story. Juan C. Cendan Tammy Y. Euliano Sergei N. Kurenov Benjamin C. Lok Related Web Sites
|