A University of Florida engineer is using advanced computer simulation techniques to come up with better knee replacements.
by Aaron Hoover Joe Kirmser was an athlete’s athlete. In high school in Connecticut he played varsity basketball and lacrosse. He went to Duke on a lacrosse scholarship, starting as goalie in four of five years. But now, at just 28, a series of injuries to his left knee have left Kirmser unable to pursue his passion for sports. “I can walk, I can ride a bike, I can swim, but I can’t run,” says Kirmser, now a master’s student in business administration at Babson College in Wellesley, Mass. “I can’t play sports. That’s pretty much done forever.” Despite
five operations, some performed by the best sports medicine surgeons in
the South, his knee remains painful and damaged. Yet he is not Kirmser is part of a small, but growing, group of people with knee injuries who are young enough to want to compete in sports but too young to make good candidates for knee replacement. So Kirmser was excited when he came across a news report about research at the University of Florida aimed at improving the durability of replacements. “I believe there’s a cure out there,” he says hopefully. It’s not a cure — not yet. But the UF research does offer hope for athletes like Kirmser as well as older people suffering from arthritis of the knee or similar problems. In a collaboration with orthopedic surgeons and engineers at other institutions, UF researchers are linking movement analysis, CT scans, computer models, computer software and other technologies to try to create longer-lasting artificial knees, improve surgical procedures and learn more about why natural knees fail. Their computer- and simulation-based approach sharply contrasts with the design-build-test paradigm still prevalent in the orthopedic industry. “More engineering analysis goes into the washing machine in your home than into the artificial knee joints in people,” says B.J. Fregly, an assistant professor of aerospace and mechanical engineering who leads the effort. “We’re changing that.”
Functional StimulationThe need for improvement is clear. More than 250,000 people receive knee replacements annually, but 68 percent of them are 65 or older, according to the American Academy of Orthopaedic Surgeons. That’s because current models tend to wear out in about 20 years, making them a poor choice for young people with serious problems caused by sports injuries or diseases such as lupus. Once a replacement wears out, options are limited. Depending on damage to the knee, surgeons can attempt a second replacement, but it is not likely to work as well as the first. A patient whose bones are too damaged to sustain a replacement has only two other options: amputation above the knee or fusion of the leg in one constant position. Also, current artificial knees have a range of motion between 110 and 120 degrees, compared to the 165 degrees of motion in natural knees. That may not sound like a big deal, but anyone who has tried living without crouching or other knee-flexing activities quickly discovers how essential those extra 50 degrees are. The problem stems in large part from the way new knee replacements are designed and tested, say Fregly and Scott Banks, who collaborates with Fregly on the UF research as technical director of the Biomotion Foundation, a West Palm Beach-based foundation dedicated to orthopedic research and education. Researchers who create new replacements typically consult orthopedic surgeons, come up with a new design and then use traditional engineering techniques to test them. The tests involve, for example, forcing the device through thousands of repetitions to ensure it will remain hardy once implanted in the body. That process takes several months and costs upwards of $40,000. “Physical testing will always be necessary,” Fregly says, “but it’s hard to get major break throughs by that approach alone.” What’s missing, Fregly says, is a step now so common as to be almost old hat in the automobile and aerospace industries and many others. “There’s no functional simulation!” he says. In other words, engineers ought to be able to design, build and test replacements all on computer, which would allow much faster testing of many more designs. “If you could provide an equivalently valid measure or prediction on computer overnight on your laptop, what an incredible tool that would be,” Banks says. That, however, is easier said than done.
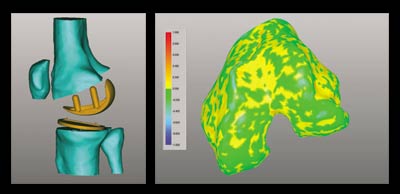
An Early Sucess Research on a potential solution starts at Banks’ laboratory in West Palm Beach. There, Banks shoots X-ray video and still photos of patients walking on treadmills or climbing stairs, both before and after knee replacement surgery. “I’m a measurement guy,” Banks says. “The end point of my process provides the raw data for B.J.’s work.” Banks ships his observations to Fregly, who relies on a multi-step computer process to model and predict the knee replacement’s movement and, more importantly, the forces it undergoes when at work in the human body. Fregly’s lab in UF’s aerospace engineering building is ground zero for the research. With anatomical charts on the walls, a half-dozen computers and samples of leg bones and artificial knee replacements on tables, the “Computational Biomechanics Lab” looks the part. The process to achieve his simulation is complex, but Fregly relies in part on a colleague in medicine, UF orthopedic surgeon Richard Vlasak. The surgeon helps ensure Fregly knows exactly how surgeons put the knee in so he’ll do the same with his “virtual” knee. “We have to balance the ligaments, or make sure that the inside ligaments are balanced and not too tight compared to the outside ligaments,” Vlasak says. “My input allows him to know what muscles and tendons are important, which ligaments we preserve and which ones we cut.” Once Fregly crafts his simulation, he ships the results to Greg Sawyer, a colleague and UF assistant professor of mechanical and aerospace engineering. In the final step in the process, Sawyer crunches the numbers to predict the actual wear on the replacement. The researchers have recently completed the first test of the simulation. In 1995, Banks shot video of a woman in her early 60s who was undergoing knee-replacement surgery. When the woman died about four years later, she donated her knee replacement back to the researchers. The researchers began working on the simulation last year and recently completed it to the point where they could see how closely it predicted the actual wear. The results were encouraging. The simulation came within a few tenths of a millimeter of predicting the wear and accurately predicted the locations of the worst wear. “That’s pretty good for the first crack,” Fregly says. The next step is to evaluate many more kinds of replacements in more people to ensure the model continues to remain accurate. “Once we do that,” Banks says, “we ought to have the ability to take new designs or modified designs and come up with predictions of how they are going to perform after years of use.” The researchers recently learned they would get some help toward that goal when the National Science Foundation announced it would award Fregly a five-year, $400,000 grant to continue pursuing the project. It was the first outside funding of the research, but not the first support for Fregly’s lab. He already has two major grants for other projects centering on the natural rather than artificial knee.
“A Beautiful Machine” Fregly says that the problem with the procedure is that surgeons essentially have to make an educated guess about how large the angle should be, with the usual figure between 7 and 10 degrees. That turns out to be correct for some people but not for others, making the results of the surgery so variable that many doctors decline to perform the operation. Fregly compares the current practice to a shoe store offering only sizes 7 to 10 shoes for adults whose foot sizes may range from 6 to 13.
“You come back the next day and say, ‘Oh, my toes are killing me, and I don’t know what it is,’ and the sales clerk scratches his head and says, ‘Gee, I can’t understand it, our population studies show that for most people, size 7 to 10 works great.’” To attack the problem, Fregly and his colleagues film patients walking in shoes, the soles of which are slanted to approximate the effects of the surgery — the shoes for a bow-legged patient, for example, forces him or her to walk knock-kneed. They then create a computer model that matches the patient’s anatomy and run tests on how closely the model “walks,” both in and out of the shoes, compared to the real patient. This step allows the researchers to correct the model by comparing its predictions to the real-world video. The final step is to have the model walk with the tibia realigned at various degrees, highlighting what the best option for surgery should be. Fregly said more data collection is needed before the project can reach the point where it will provide recommendations for surgeons. The project is funded by the Whitaker Foundation. Fregly’s third project probes the causes of knee arthritis itself — an area that has long proven mysterious because it is so difficult to determine what is happening inside the knee as a person walks. The team is seeking to predict inner forces on the knee using computer models, CT scans and reverse-engineering software. One result of the three-year project, funded with a $210,000 grant from the National Institutes of Health, may be a better understanding of how to guard against arthritis. Vlasak, the orthopedic surgeon, said working with Fregly and the other researchers offers him a rare opportunity to go beyond treating patients and improve orthopedics as a whole. And with his engineering background, Fregly brings a lot to the table, he says. “As orthopedic doctors go, we tend to think of the human being as a machine, but a beautiful machine,” he said. “Working with an engineer who understands man-made machines, I think he’s better able to appreciate the intricacies of a machine made by God.”
|
 |
|
|
RGP Home
| Sponsored Research
| Graduate Education
| Technology Licensing Administrative Services | Research Communications | Contact the Webmaster |